Stress is often painted with a broad, negative brush, but not all stress is created equal. In the realm of stress science, we distinguish between eustress (good stress) and distress (bad stress), each with its unique impact on our health and well-being. While distress can feel overwhelming and harmful, eustress plays a surprisingly positive role in motivation, focus, and even personal growth.
Let’s break down the science of stress, what separates helpful stress from harmful stress, how it affects your body and mind, and how you can build resilience through practices that support your nervous system.
What is Good Stress? Understanding Eustress and Its Benefits
Not all stress is harmful. Eustress, or positive stress, is the type that energizes us, sharpens focus, and supports personal growth. It typically arises in short bursts during situations we perceive as challenging but manageable. Whether it’s prepping for a big presentation or pushing yourself during a workout, eustress can help you perform at your best.
These short-term, controlled stressors, also referred to as hormetic stressors, train the body to adapt to physiological changes and return to a calm, regulated state. This process strengthens your stress response over time, particularly through the activation of the vagus nerve, which plays a central role in calming the body after stress.
Common Examples of Eustress:
♥️ Going on a first date
📆 Meeting a tight work or school deadline
💼 Starting a new job
✍ Preparing for a speech or big event
🏃🏻♀️ Exercising just beyond your comfort zone
Benefits of Eustress:
- Improved performance: Enhances focus and productivity through controlled activation of the sympathetic nervous system and the release of norepinephrine.
- Increased motivation: Boosts drive and goal-setting behavior through dopamine signaling.
- Greater stress resilience: Builds your body’s capacity to adapt to future stressors by strengthening the nervous system’s ability to recover.
What is Bad Stress? Understanding Distress and Its Impact
On the flip side of eustress is distress, the harmful form of stress that can negatively affect both physical and mental health, especially when it’s intense, prolonged, or left unmanaged.
Distress overwhelms the body’s ability to cope and regulate. It keeps the sympathetic nervous system in a heightened state of arousal, reduces vagus nerve activity (vagal tone), and can contribute to serious health conditions over time.
Common Causes of Distress:
- Chronic stressors like toxic work environments, relationship conflict, or financial instability
- Traumatic events, such as adverse childhood experiences, abuse, or being a victim of violence
- Major life changes, including divorce, the loss of a loved one, or serious illness
These experiences can lead to HPA axis dysregulation and reduced vagal tone, leaving the body stuck in “fight or flight” mode and impairing its ability to return to a calm, regulated state.
Health Conditions Associated with Chronic Distress:
- Migraines and cluster headaches
- Digestive disorders (e.g., IBS)
- Insomnia and disrupted sleep
- Chronic pain and inflammation
- Anxiety, depression, and mood disorders
- Cognitive decline and memory issues
The Physiology of Stress: What’s Happening in Your Body
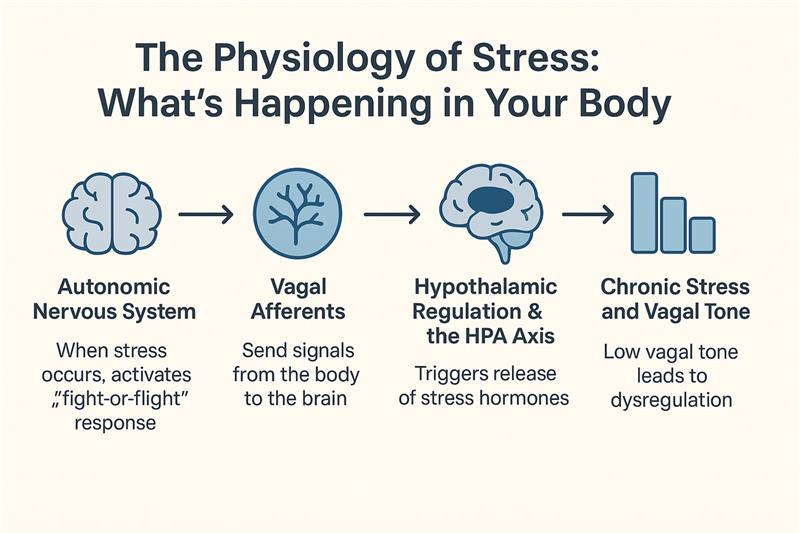
Whether you’re experiencing good stress (eustress) or bad stress (distress), your body responds through a sophisticated system designed to help you adapt and survive. This response involves both the autonomic nervous system and the hypothalamic-pituitary-adrenal (HPA) axis, your body’s core stress-response pathway.
At the center of this system is the vagus nerve, which is made up mostly of afferent (sensory) fibers. These fibers detect internal changes, like inflammation or shifts in metabolism, and send signals from the body to the brain, where they reach the brainstem and the hypothalamus, the part of the brain that controls the release of stress hormones.[1]
Let’s take a closer look at how this all works together:
- Autonomic Nervous System
When a stressor is detected, the sympathetic nervous system (part of the autonomic nervous system) kicks into gear. It triggers the classic “fight-or-flight” response: increased heart rate, heightened alertness, immune system activation, and a rise in inflammation, which is designed to help your body respond to a perceived threat.
Once the stressor is gone, the parasympathetic nervous system, largely regulated by the vagus nerve, works to bring the body back to a calm, regulated state. This balance between sympathetic activation and parasympathetic recovery is crucial for overall health.
- Vagal Afferents: Body-to-Brain Signaling
As these internal shifts occur, the vagus nerve’s afferent fibers pick up on them and send signals to the nucleus of the solitary tract (NTS) in the brainstem.[2] This is where the brain begins to assess the body’s internal state and determine the appropriate stress response.
- Hypothalamic Regulation & the HPA Axis
From the NTS, information is passed to the hypothalamus, which then activates the HPA axis, a hormonal cascade that further amplifies the stress response by releasing:
- CRH (Corticotropin-Releasing Hormone)
- ACTH (Adrenocorticotropic Hormone)
- Cortisol, the body’s primary stress hormone, which influences energy levels, inflammation, blood pressure, and sleep/wake cycles.[1][3]
This system helps your body cope with immediate stressors, but only for so long.
- Chronic Stress and the Role of Vagal Tone
When stress becomes chronic, this entire system can become dysregulated, especially the HPA axis. Over time, elevated cortisol and low vagal tone can lead to inflammation, poor sleep, anxiety, and a host of physical and mental health issues.[1]
However, higher vagal tone, a sign of a well-functioning parasympathetic system, has been linked to better stress resilience and faster recovery.[4][7]
Research shows that vagus nerve stimulation (VNS) can help rebalance the system by modulating activity in the paraventricular nucleus (PVN) of the hypothalamus, which plays a key role in regulating the HPA axis.[3][4][5][6] When vagal tone is strong, your body is better able to turn off the stress response, reduce inflammation, and return to a regulated state.[7]
Hormesis: Building Resilience Through Good Stress
Hormesis is the idea that small amounts of controlled stress can actually be good for you, helping your body become stronger, more adaptable, and better able to handle future stress.
Here are a few examples of positive stress that can boost resilience:
- Exercise: Regular movement puts healthy pressure on the body, improving strength, endurance, and stress recovery.
- Intermittent Fasting: Short periods without food can help your body become more efficient and balanced.
- Temperature Exposure: Brief exposure to heat (like a sauna) or cold (like a cold shower) can help your body adjust more easily to physical and emotional stress.
Understanding the difference between good stress and bad stress is key to taking care of your mind and body. By building up your body’s stress recovery system, through things like deep breathing, yoga, vagus nerve stimulation, and controlled exposure to positive stress, you can become more resilient, feel more balanced, and support your long-term health.
Ready to support your vagus nerve and build lasting resilience? Explore how Truvaga can help.
Sources:
- Varela, Sofia, Amanda M. Shelton, Jake A. Montgomery, et al. 2023. “Neural Regulation of the Stress Axis: The Many Faces of Stress.” Frontiers in Endocrinology 14:1103621. https://www.frontiersin.org/articles/10.3389/fendo.2023.1103621/full
- Cleveland Clinic. 2022. “What Does the Vagus Nerve Do?” Cleveland Clinic Health Essentials, November 1. https://health.clevelandclinic.org/what-does-the-vagus-nerve-do
- Ulrich-Lai, Yvonne M., and James P. Herman. 2009. “Neural Regulation of Endocrine and Autonomic Stress Responses.” Nature Reviews Neuroscience 10(6):397–409. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4867107/
- Integrative Therapies and Wellness. 2021. “The Vagus Nerve and Hormones.” IntegrativeTherapiesandWellness.com, September 15. https://www.integrativetherapiesandwellness.com/blog/the-vagus-nerve-and-hormones
- Gold, Lucie. 2021. “Vagus Nerve Stimulation Modulates the HPA Axis via Hypothalamic Circuitry.” bioRxiv, June 3. https://www.biorxiv.org/content/10.1101/2021.06.03.446790.full
- Gold, Lucie. 2021. “Vagus Nerve Stimulation and Hypothalamic Regulation: Initial Preprint Release.” bioRxiv, June 3. https://www.biorxiv.org/content/10.1101/2021.06.03.446790v1
- Massachusetts General Hospital. 2022. “Mass General Research Sheds Light on the Vagus Nerve’s Role in Health.” MassGeneral.org, October 3. https://www.massgeneral.org/news/article/vagus-nerve
- Mouton, P. R., Long, J. M., Lei, D. L., et al. 2022. “A Review of the Role of Vagus Nerve Stimulation in Modulating the Brain–Gut Axis.” International Journal of Molecular Sciences 23(17):9881. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9405171/
Author bio:
Dr. Navaz Habib, is the bestselling author of “Activate Your Vagus Nerve,” and the newly released “Upgrade Your Vagus Nerve.” He is also the host of “The Health Upgrade Podcast.”
After graduating as class valedictorian from Canadian Memorial Chiropractic College in 2010 and went on to practice traditional chiropractic for years, until he utilized the power of functional medicine to transform his own health. Dr. Habib is the founder of “Health Upgraded” an online functional health consulting clinic, supporting optimal health by elevating the awareness and function of the vagus nerve.