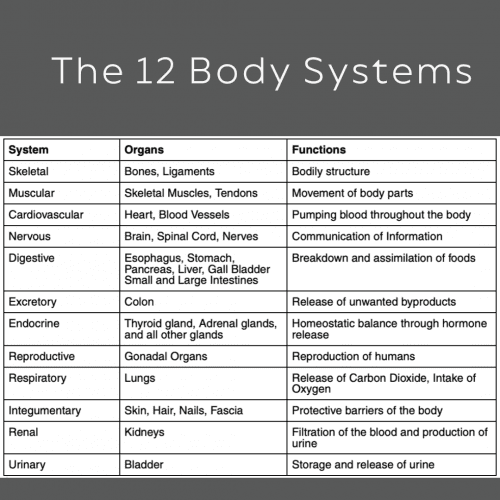
For the past hundreds of years in medicine, we have worked to separate the body into separate sections called systems and further broken down these systems into organs. It’s important to understand the underlying and unique functions of each of the cells and organs in each system to provide a deeper understanding of the particular needs of each cell, organ, and system.
But we must remember that the body only works as a whole and that each of these cells, organs and systems need to communicate with one another to ensure the optimal holistic function of the body. We have 12 main body systems that need to communicate and work like a beautiful, harmonious symphony.
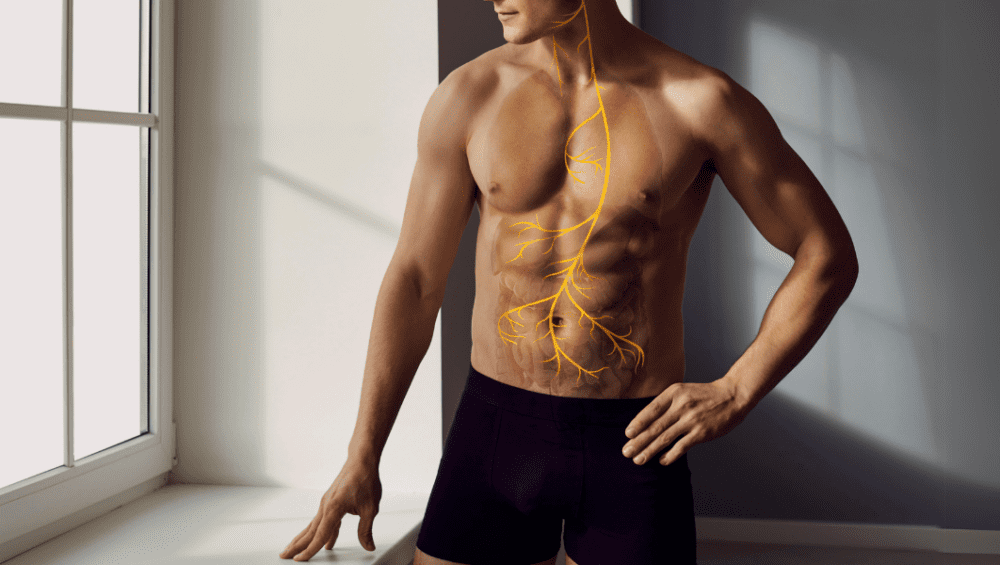
One of the main ways that these body systems work in unison is through effective communication. The most effective method of communication between these 12 systems we have in our bodies is the vagus nerve!
What is the vagus nerve?
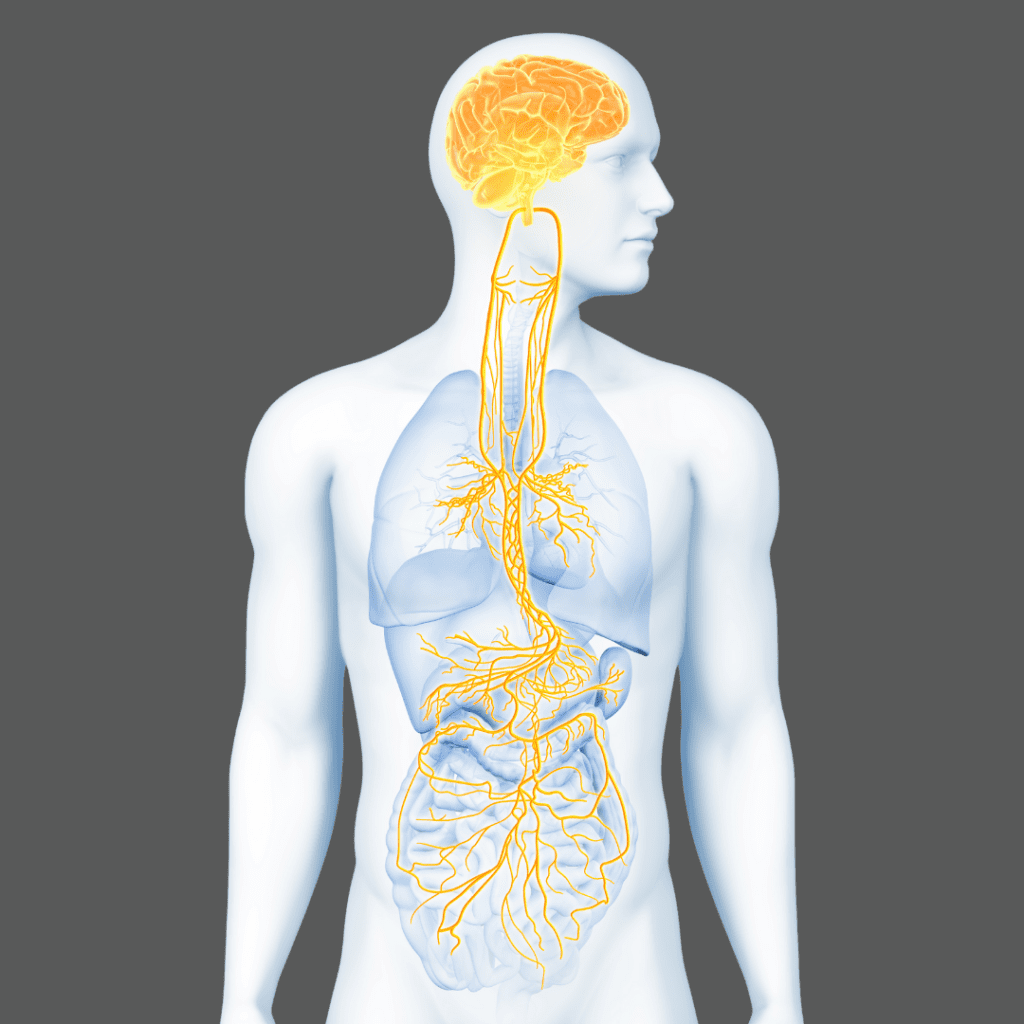
The vagus nerve is the 10th and longest cranial nerve that connects our body and brain, helping the brain communicate with the 12 main body systems. It’s the uniting structure to ensure the synergistic function of all the unique happenings underlying our optimal function.
We have 12 pairs of cranial nerves that sense and control functions in and around the face and head. The vagus nerve is the 10th of these 12 nerves, and it comes in a pair (one on each side of the body). It’s important to note that the vagus nerve is the only cranial nerve that leaves the head and neck area!
Where does the vagus nerve journey start?
The physical vagus nerve begins when it branches off the brainstem on either side of the body from a region called the medulla oblongata, then sends its initial branches to areas of the head and neck.
The first branch is called the auricular branch and is connected to the skin of the auricle of the ear. This branch sends sensory information from a section of the auricle (the visible part of the ear) to the brainstem. This is the vagus nerve’s direct connection to the integumentary system, but there are only about 800-1000 nerve fibers from the vagus nerve that connect to this area, a very low number in relation to the nerve itself (only 1% of the information on vagus comes from this branch).
The next branches are the pharyngeal and laryngeal branches. These branches are connected to muscles located in the airway and around the vocal cords. Signals sent on these branches go from the brain to these muscles to ensure that our airways remain open and unobstructed. This allows us to breathe and vocalize with pitch and tone by tensioning and releasing pressure on the vocal cords. These branches are how the vagus nerve connects directly to the muscular system.
Vagus nerve access at the neck
The vagus nerve then continues down in the neck within a protective layer of tissue known as the carotid sheath, along with two VERY important blood vessels on either side – the carotid artery and the jugular vein. These blood vessels are imperative for effective blood flow to and from the brain, so this is a major clue as to the importance of these three structures (Carotid artery, jugular vein and vagus nerve) within the carotid sheath.
The region in the neck where the vagus nerve is located happens to be where the vagus nerve is most easily accessible within the body. Therefore, this is a great spot to stimulate the vagus nerve using electric stimulation. The area where you feel your carotid pulse in your neck (both sides) is within just 1.3 cm below the skin’s surface near the thickest part of the vagus nerve, and this is why Truvaga is directed at these fibers in the neck.
Next stop, the thorax
Once the nerves enter the thorax (internal chest area), the left and right sides intertwine and become meshed together around the esophagus and trachea, then begin to send branches to many of our internal organs.
In the thorax, the vagus nerve branches directly to the heart to control heart rate and send parasympathetic signals. This is one area where it connects to the cardiovascular system.
Also, within the thorax are many branches that break off and go to the lungs (respiratory and immune systems) to send and receive signals about what is happening in the lungs regarding all aspects of breathing and the function of the immune cells in the lungs, thus being connected to the respiratory system.
Where does the vagus nerve end?
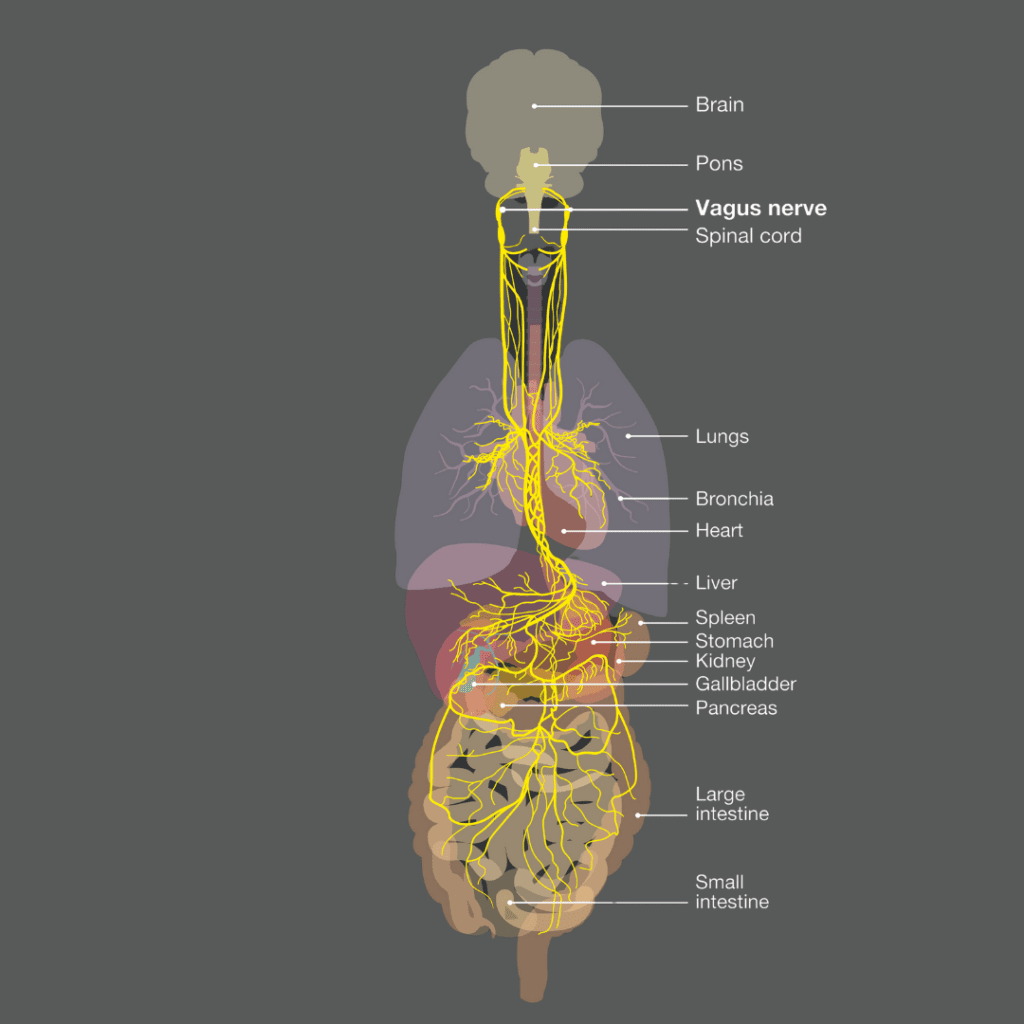
The main trunks of the vagus nerve continue down along the esophagus and pass through the diaphragm muscle to enter the abdomen (belly area). Within the abdomen, the vagus nerve sends branches off to connect directly with essentially every visceral organ, including
- Stomach (digestive system)
- Pancreas (digestive system)
- Liver (digestive and excretory systems)
- Gall bladder (digestive and excretory systems)
- The entire length of the small intestine (immune and digestive systems) including all three sections
- Ascending colon and part of the transverse colon (immune, digestive, and excretory systems)
- Kidneys (urinary system)
- Indirectly to the spleen (a very important connection that signals how we control inflammation and immune system function throughout the body)
The remainder of the lower intestinal tract, bladder, and genital organs are innervated with parasympathetic signals coming from nerve branches from the sacral region.
Body-to-brain communication
What makes the vagus nerve so unique is that there is no other nerve in the body with such extensive direct connections to so many organs and tissues.
Another very important thing to understand is that the vast majority of information being passed on the vagus nerve actually comes from these organs, up to the brainstem, and ultimately into the brain for processing. In fact, over 80% of the information on the vagus nerve is sent in this direction, which is called afferent (from the body to the brain).
One of the unique functions that these afferent vagus nerve signals support is a process called ‘Interoception,’ literally the sensation of how things are working within our bodily organs. While this sense is not as specific as touch, taste, and sight, it is something you have certainly experienced at some point in your life.
If you have ever noticed that your digestion was off, you felt bloated, noticed an elevated heart rate or pounding of your pulse, and even the sensations of being dehydrated, you have experienced interoception.
Without these vagus nerve signals being sent up to the brain, we are unable to fully grasp the current status of our internal functions. Dysfunctional interoception has been linked to many mood and affect disorders, so these are very important signals that need to make their way up to the brain.
Microbiome gut-brain axis
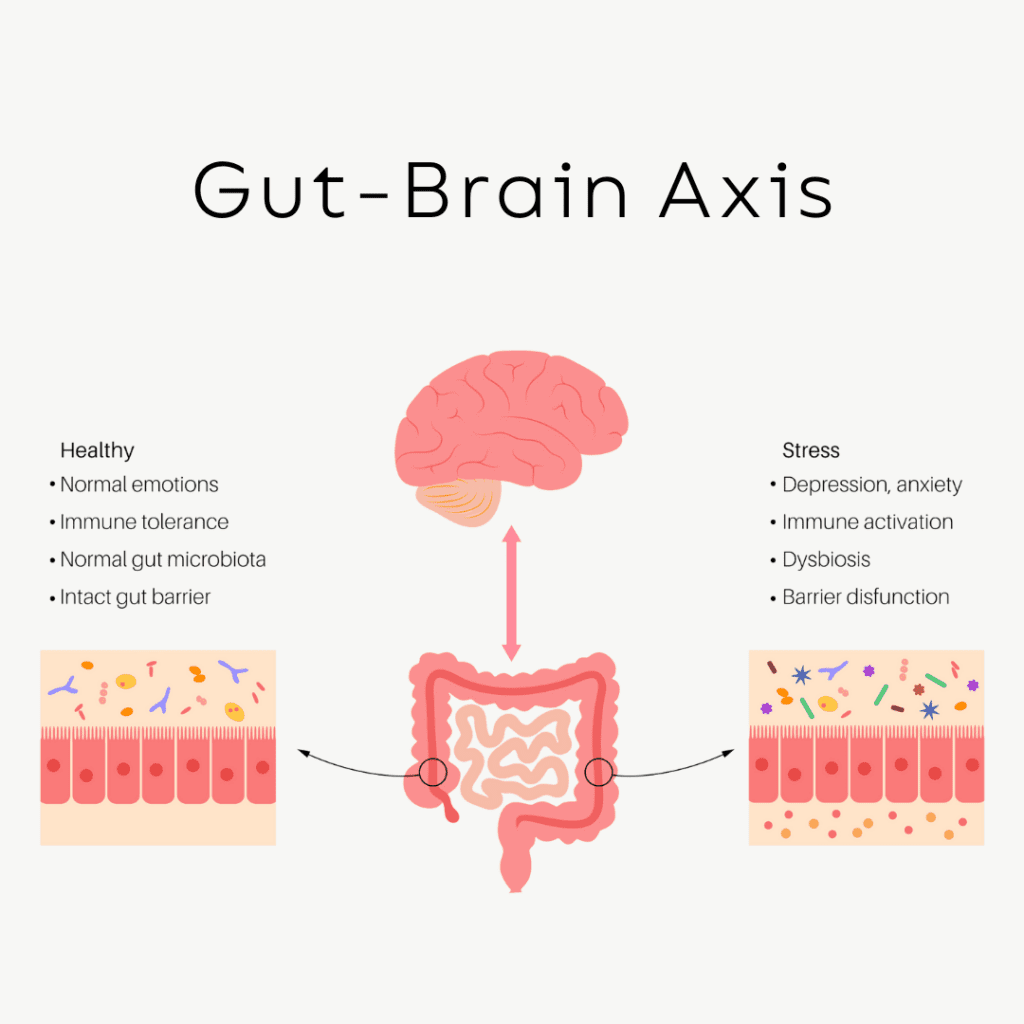
Another component of the signals that make their way up to the brainstem through these afferent signals are signals from the microbiome through what is called the Microbiome-Gut-Brain axis. Humans have between 80 to 100 trillion bacteria located in our intestinal tracts, that we need to have a symbiotic relationship with.
These bacteria produce many important biochemicals that help us function optimally, including short-chain fatty acids like butyrate and precursors to the important neurotransmitters serotonin and dopamine.
Dysbiosis is the term given to a less-than-optimal balance of bacteria, parasites, viruses, yeast and worms that are living in our gut, and dysbiosis is one of the most overlooked causes of chronic inflammation that we see today. An effective and strong vagus nerve is a necessity in order to ensure that our bodies don’t go down this inflammatory pathway and lead to dysfunction or even disease.
Brain-to-body communication
About 15% of the information passed along the vagus nerve is called efferent parasympathetic information, meaning that its signals are coming from the brainstem to the body organs. These signals are sent to their respective systems that regulate the function of the immune system.
Immune system cells are located in every single organ throughout the body. This system has historically been believed to only have the function of protecting us from threats to survival. While this is one major function of the immune system, it also has many other very important functions.
The innate immune cells located in each organ, called tissue-resident macrophages, are the regulatory cells that support the building of each organ during development. They remain in these organs throughout our lives, ensuring that the organs perform their respective functions at a high level. They function in much the same way that the security, housekeeping, and maintenance staff function in a hotel.
Efferent signals from the vagus nerve regulate the function of cells located in each organ, ensuring that each system and organ maintains a great functional status as long as possible. This path is called the Cholinergic Anti-Inflammatory Pathway and was discovered by Dr. Kevin Tracey and his team at the Feinstein Institute in the late 1990s and early 2000s.
In summary
It is quite clear that there is no other nerve in the body quite as extensive in its connections and functions as the vagus nerve. Understanding the anatomy, system and organ connections of this nerve helps us to gain an understanding as to why vagus nerve stimulation can be so powerful as a tool to help us feel calmer, think clearer, and sleep better.
Truvaga is a great choice to help you regulate the function of this nerve, ensuring that important signals get to and from the brain and the body.
Author bio:
Dr. Navaz Habib, is the bestselling author of “Activate Your Vagus Nerve,” and the newly released “Upgrade Your Vagus Nerve.” He is also the host of “The Health Upgrade Podcast.”
After graduating as class valedictorian from Canadian Memorial Chiropractic College in 2010 and went on to practice traditional chiropractic for years, until he utilized the power of functional medicine to transform his own health. Dr. Habib is the founder of “Health Upgraded” an online functional health consulting clinic, supporting optimal health by elevating the awareness and function of the Vagus nerve.